Tresiba (insulin degludec) and Basaglar (insulin glargine) are both long-acting insulins used to manage blood glucose levels in people with diabetes, but they have key differences in formulation, duration, and usage. Here’s a breakdown:
- Type of Insulin
• Tresiba: Contains insulin degludec, an ultra-long-acting insulin.
• Basaglar: Contains insulin glargine, a long-acting insulin.
- Duration of Action
• Tresiba: Provides glucose control for up to 42 hours with consistent, steady action. This allows for flexible dosing, meaning it doesn’t have to be taken at the same time every day (as long as there’s at least 8 hours between doses).
• Basaglar: Works for approximately 24 hours. It is typically taken once daily at the same time each day for optimal control.
- Onset of Action
• Tresiba: Starts working in about 1 hour.
• Basaglar: Takes about 1-2 hours to start lowering blood sugar.
- Flexibility in Dosing
• Tresiba: Offers more flexibility in administration time due to its ultra-long action.
• Basaglar: Requires stricter adherence to a consistent schedule.
- Concentration
• Tresiba: Available in two concentrations — U-100 and U-200.
• Basaglar: Available only as U-100.
- Patient Suitability
• Tresiba: Ideal for patients who need flexibility or have issues adhering to strict dosing schedules.
• Basaglar: Suitable for those who can follow a consistent schedule.
- Cost and Insurance Coverage
• Basaglar: Considered a “follow-on” biologic (similar to a biosimilar), it’s often less expensive and may be preferred by insurance plans.
• Tresiba: A newer insulin, typically more expensive but may be covered depending on the insurance.
- Approval and Use
• Tresiba: Approved for both adults and children as young as 1 year old with type 1 or type 2 diabetes.
• Basaglar: Approved for adults and children as young as 6 years old with type 1 diabetes and adults with type 2 diabetes.
Information about Tresiba’s flexibility and no insulin stacking worry:
The 42-hour duration of Tresiba doesn’t mean each dose lasts precisely 42 hours in your body. Instead, it reflects its ultra-long-acting profile, which ensures stable blood sugar control even if doses are not perfectly timed. Here’s how it works:
Key Points of Tresiba’s Dosing Flexibility:
- Overlapping Action:
Tresiba maintains steady insulin levels because doses overlap. When you take a new dose, it adds to the residual effects of the previous dose. This overlap creates a consistent baseline level of insulin in your bloodstream.
- Minimum Time Between Doses:
While Tresiba lasts up to 42 hours, you only need at least 8 hours between doses because:
• A new dose contributes to the overall insulin level without causing a peak.
• The ultra-long action ensures no significant drop in blood sugar coverage, even with flexible timing.
- Consistency in Dosing:
For optimal results, Tresiba is designed to be taken once daily, but it doesn’t have to be at the same time every day. For example:
• If you take Tresiba at 8 a.m. today, you could take it as early as midnight tonight or as late as 2 p.m. tomorrow, depending on your schedule.
• This flexibility is helpful for shift workers, travelers, or those who struggle with strict schedules.
- Why You Don’t Need to Wait 42 Hours:
Each dose of Tresiba contributes to a steady insulin reservoir in your body. This reservoir ensures consistent blood sugar control regardless of slight timing changes. The long duration simply provides a safety net, not a reason to delay dosing.
Practical Example:
• Day 1: Dose at 8 a.m.
• Day 2: Dose at 11 p.m. (15 hours later)—this is fine because the 8-hour minimum has been met, and the previous dose is still active.
• Day 3: Dose at 9 a.m. (10 hours later)—again, no problem because of the overlap.
Takeaway:
While Tresiba lasts a long time, its dosing schedule is designed to prioritize convenience and consistency rather than strict timing. You’re not “starting from scratch” with each dose; you’re topping up your body’s steady insulin level. Always consult your healthcare provider for personalized guidance on adjusting your schedule.
As far as overlapping and insulin stacking:
Great question! No, you’re not adding too much insulin to your body when doses of Tresiba overlap. Here’s why:
- Tresiba’s Steady Release Mechanism
• Tresiba (insulin degludec) is designed to release very slowly and evenly into the bloodstream. Unlike rapid-acting insulin, it doesn’t create peaks in insulin levels.
• Even when doses overlap, the combined insulin effect remains smooth and stable without sudden increases.
- Why Overlap Doesn’t Cause “Too Much Insulin”
• Each dose of Tresiba contributes to a baseline insulin level, and the total amount in your body is designed to stay within a safe and therapeutic range.
• Tresiba’s ultra-long half-life (about 25 hours) ensures that the insulin degrades gradually, preventing a buildup.
- Built-in Safety Mechanism
• Tresiba’s dosing flexibility has been extensively studied. The overlap was found to be safe and effective in managing blood glucose levels without increasing the risk of hypoglycemia (low blood sugar).
• Even if you dose earlier or later than usual, the insulin levels in your body adjust to provide steady coverage.
- How Overlap is Accounted For
• The total daily dose you take is calculated based on your body’s insulin needs over 24 hours. When you “top up” with a new dose, you’re maintaining this baseline level, not doubling up or creating excess insulin in your system.
- Monitoring is Key
• While Tresiba is very forgiving, it’s still important to work with your healthcare provider to determine the correct daily dose and to monitor your blood glucose levels. This ensures your insulin needs are met without any risk of overcorrection.
Summary
The overlap of Tresiba doses works by design and does not lead to excessive insulin because of its slow, steady action and the way it is metabolized. As long as you follow your prescribed dose and timing guidelines, it’s highly unlikely to cause problems with overlapping doses. If you ever notice low blood sugar symptoms, consult your healthcare team to fine-tune your dosing.
If dose needs to be higher:
If you need to increase your Tresiba (insulin degludec) dose, it should be done gradually and carefully, based on your blood glucose patterns and guidance from your healthcare provider. Here’s how dose adjustments are typically handled:
- When to Consider an Increase
You might need to increase your Tresiba dose if:
• Your fasting blood sugar (morning blood sugar) is consistently higher than your target.
• Your blood glucose levels are persistently elevated throughout the day, despite following your meal plan and using any other insulin or medications appropriately.
- How to Safely Adjust the Dose
• Small Increments: Dose increases are usually made in small steps, such as 1–4 units at a time, depending on your needs and your provider’s advice.
• Timing of Adjustments: Make adjustments after observing your glucose trends for 3–4 days (not based on a single high reading).
• Monitor Closely: Check your fasting glucose and overall trends more frequently when increasing your dose to ensure you’re staying within your target range without risking low blood sugar (hypoglycemia).
- The Role of Overlap in Dose Increases
When increasing your Tresiba dose:
• The steady, overlapping action of Tresiba ensures that the dose change affects your overall baseline insulin level evenly.
• Since Tresiba doesn’t peak, an increase will result in a slightly higher, but still stable, insulin level throughout the day and night.
- Practical Example
• Current dose: 20 units/day
• Fasting glucose trend: 140–160 mg/dL (above your target of 90–130 mg/dL)
• Adjustment: Increase to 22 units/day.
• Monitor: Check fasting blood glucose for the next 3–4 days to see if it drops closer to the target range.
- When to Stop Increasing
• If your fasting blood glucose reaches your target range.
• If you experience hypoglycemia (low blood sugar). In this case, the dose might need to be lowered slightly.
- Talk to Your Healthcare Provider
Your provider might recommend additional strategies, such as:
• Adjusting your mealtime insulin (if applicable).
• Reviewing your diet, exercise, or other factors that might affect glucose levels.
Key Takeaway
Tresiba’s flexibility makes dose adjustments safe and manageable. However, because it’s long-acting, changes take a few days to show their full effect, so adjust cautiously and monitor closely. Always consult your healthcare provider when making significant changes to your insulin regimen.
How Basaglar is different and not flexible and can cause insulin stacking if doses overlap:
No, Basaglar (insulin glargine) does not work the same way as Tresiba (insulin degludec) in terms of dose overlap and flexibility. Here’s how Basaglar differs:
- Duration of Action
• Basaglar lasts about 24 hours, but this duration can vary slightly depending on the individual.
• Unlike Tresiba, which can last up to 42 hours, Basaglar provides less “wiggle room” for overlapping doses.
- Dosing Schedule
• Strict Timing: Basaglar should be taken at the same time every day to maintain consistent insulin levels.
• Taking it earlier or later than usual could result in gaps in coverage or stacking of insulin, which can increase the risk of high or low blood sugar.
- Overlap of Doses
• Basaglar’s steady action over 24 hours means there’s little flexibility for overlapping doses. If you take a second dose less than 24 hours after the first, you may risk stacking insulin, which could lower blood sugar levels more than intended (causing hypoglycemia).
• It is important to wait at least 24 hours between doses unless your healthcare provider advises otherwise.
- Why Basaglar Isn’t as Flexible
• Half-Life: Basaglar has a shorter half-life compared to Tresiba, so it clears from the body faster.
• Peak-Like Effect: While Basaglar is considered “peakless,” some individuals experience a slight peak in action 4–6 hours after injection, making overlapping doses more likely to result in hypoglycemia.
- What to Do if You Miss a Dose
• If you miss a dose of Basaglar, take it as soon as you remember, as long as it’s not too close to the next scheduled dose. If it is, skip the missed dose and resume your normal schedule.
• Never take two doses of Basaglar within 24 hours without medical advice.
Summary
While Tresiba is designed for flexible dosing and overlap, Basaglar is less forgiving due to its shorter duration and lack of overlapping design. Stick to a consistent daily schedule with Basaglar and consult your healthcare provider if you need to adjust your timing.
How Tresiba works:
Tresiba (insulin degludec) doesn’t create an issue with insulin stacking because of its unique pharmacokinetics—the way it works in the body. Here’s why:
- Ultra-Long and Steady Action
• Tresiba has an ultra-long duration of action (up to 42 hours), which ensures a smooth, stable release of insulin into the bloodstream over time.
• Instead of peaking like some insulins, Tresiba maintains a flat, steady profile, meaning it doesn’t cause fluctuations in insulin levels even if doses overlap slightly.
- Low Daily Accumulation
• Tresiba has a half-life of about 25 hours, meaning only a portion of the previous dose remains in your system when you take your next dose.
• When taken daily, the insulin reaches a steady-state level in the body after a few days. At this point, overlapping doses combine to maintain a consistent baseline rather than accumulating excessively.
- Molecular Design
• Tresiba forms multihexamers under the skin after injection, which slowly and predictably release insulin over time.
• This gradual release prevents insulin levels from spiking or stacking, even when doses are taken less than 24 hours apart.
- Flexibility is Built Into Its Design
• Tresiba was specifically developed to allow for dosing flexibility. Studies show that taking doses at different times (as long as there’s an 8-hour gap) doesn’t cause hypoglycemia or excessive insulin accumulation.
• The overlap simply maintains the steady insulin baseline needed for glucose control.
- How This Differs from Other Insulins
• Basaglar and similar insulins: These have shorter durations (about 24 hours) and can exhibit mild peaks, making overlapping doses more likely to cause stacking and hypoglycemia.
• Tresiba’s ultra-long profile avoids this problem by ensuring insulin depletes at the same rate it’s being added, keeping levels consistent.
Example of Safe Overlap
• Day 1: Dose at 8 a.m.
• Day 2: Dose at 11 p.m. (15 hours later)
• The dose given on Day 1 is still active but is steadily tapering off. The new dose takes over, smoothly maintaining the overall insulin level.
• This flexibility ensures you can adjust the timing without stacking too much insulin.
Key Takeaway
Tresiba’s slow, steady release and ultra-long action prevent insulin stacking by creating a seamless overlap between doses. This unique property sets it apart from other long-acting insulins, making it safer and more flexible.
Popularity:
Both insulin glargine (like Lantus, Semglee, and Basaglar) and insulin degludec (like Tresiba) are commonly used long-acting insulins for type 1 diabetes, but insulin degludec (Tresiba) has been gaining popularity in recent years for a few key reasons.
- Duration of Action
• Insulin Glargine (Lantus, Semglee, Basaglar): Typically provides a 24-hour coverage. Some people find it requires more frequent adjustments, especially if their insulin needs vary during the day or if they have fluctuating blood sugar levels.
• Insulin Degludec (Tresiba): Has an ultra-long duration of up to 42 hours, which offers more flexibility in terms of timing. Many people find this helpful for reducing the complexity of insulin dosing and minimizing the risk of missed doses.
- Dosing Flexibility
• Insulin Glargine: Must be taken at roughly the same time each day to maintain consistent blood sugar control, making timing more important.
• Insulin Degludec: Allows for more flexibility, with dosing windows up to 8 hours apart, making it more convenient for people with busy or unpredictable schedules.
- Stable Blood Sugar Control
• Insulin Glargine: Although considered a “peakless” insulin, it can still cause some variability in blood sugar levels for some people due to its action profile.
• Insulin Degludec: Is known for its smooth and steady release, with very minimal variability, which can lead to more consistent blood sugar levels for many people.
- Hypoglycemia Risk
• Insulin Glargine: While it’s designed to have minimal peaks, some users still report a higher incidence of nighttime hypoglycemia, especially if their blood sugar drops while they’re asleep.
• Insulin Degludec: Because of its ultra-slow and steady release, it tends to have a lower risk of hypoglycemia, particularly nocturnal hypoglycemia, which is a common concern for many type 1 diabetics.
- Patient Preference and Popularity
• Insulin Glargine: It has been the standard for many years, and many patients still prefer it due to familiarity and long-term use. It’s generally well-tolerated and has a well-established track record.
• Insulin Degludec: Tresiba is becoming increasingly popular because of its flexibility, convenience, and longer duration of action. Studies have shown that people using Tresiba experience better glucose control and fewer incidents of hypoglycemia compared to insulin glargine.
Conclusion:
While insulin glargine remains a popular choice for type 1 diabetes and has been in use for longer, insulin degludec (Tresiba) is becoming more popular, especially for those seeking greater flexibility, consistent blood sugar control, and a reduced risk of hypoglycemia. Many type 1 diabetics who switch to Tresiba find it better fits their lifestyle, particularly in managing unpredictable schedules or improving overall control. However, the choice between the two still depends on individual needs, preferences, and how a person’s body responds to each insulin.
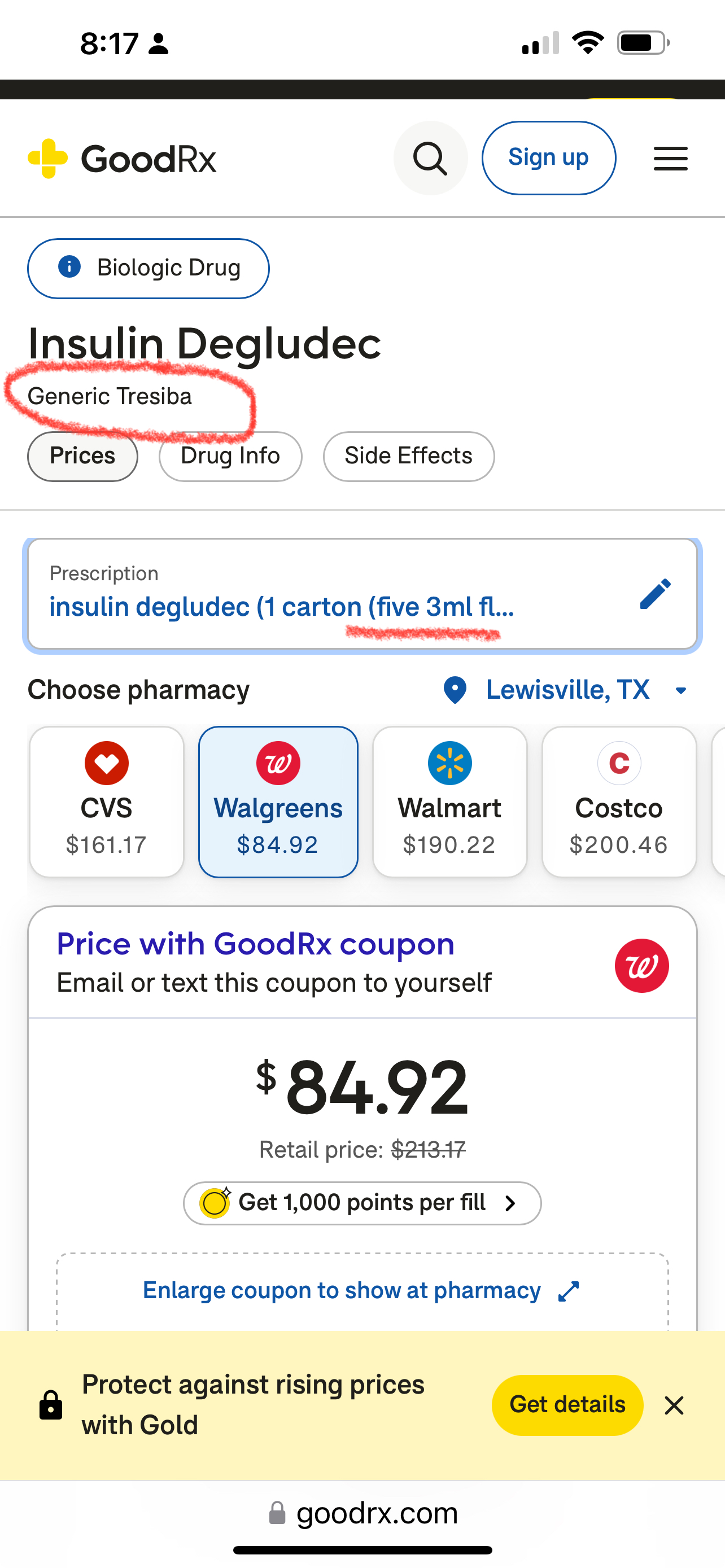
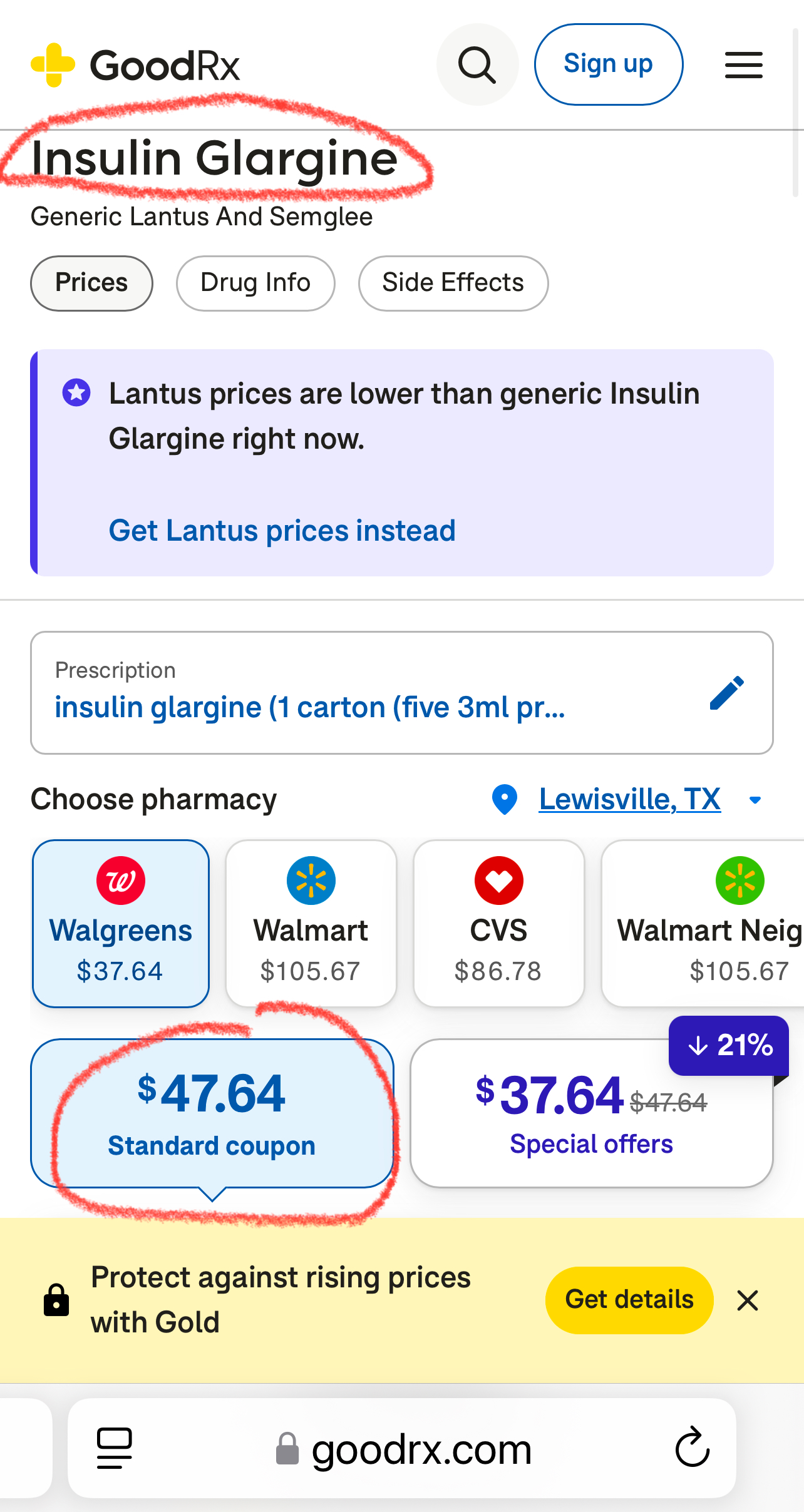
Generic Tresiba (insulin Degludec) with GoodRx coupon is not expensive for a box of 5 pens. Always check Goodrx against insurance price and ask for generic whenever possible. The Brand name Tresiba price was over $530 with coupon. I don’t know the insurance price but probably still a lot compared to generic insulin with coupon.
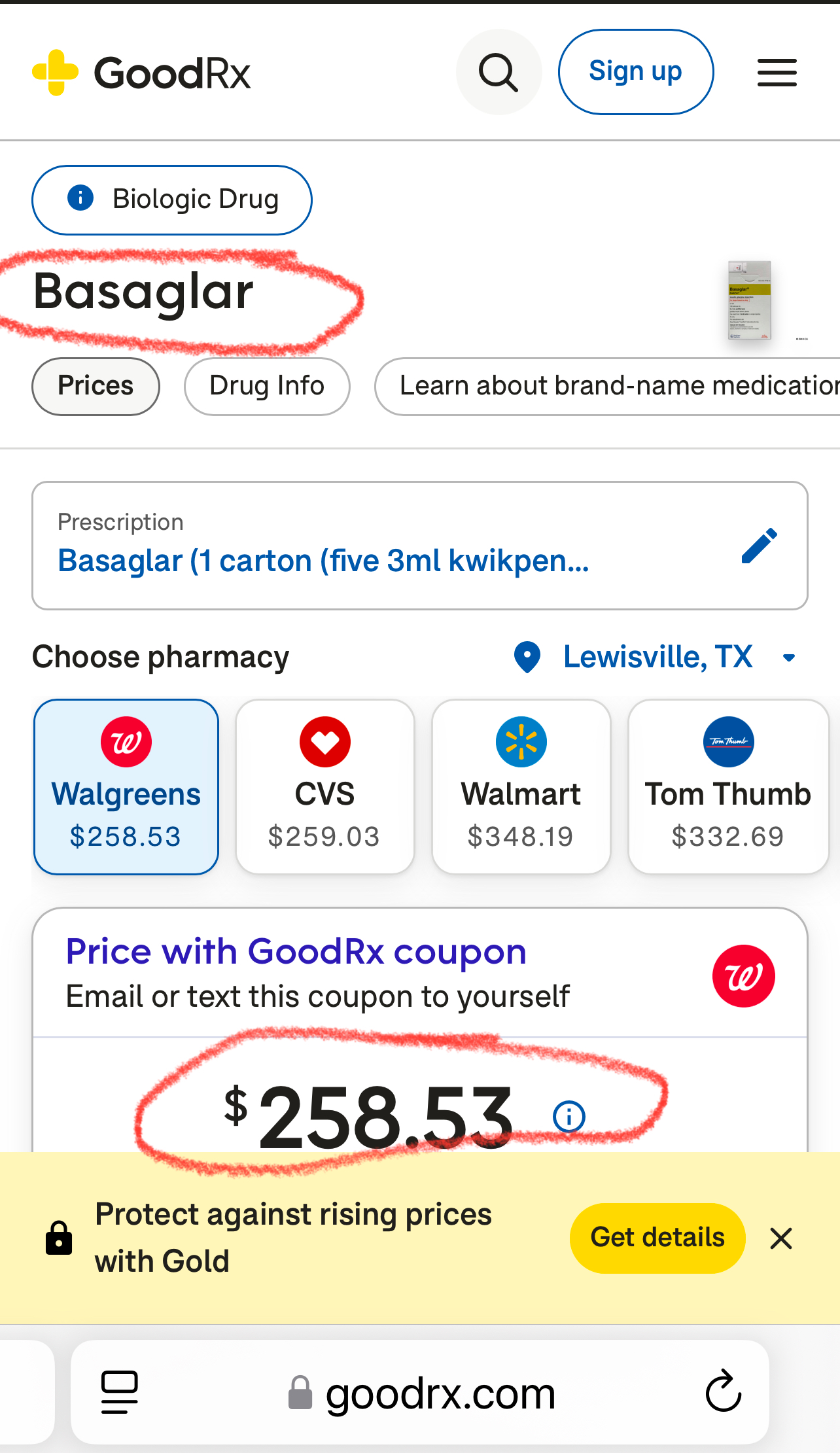
The insulin Glargine like Basaglar is less expensive but higher risks. Goodrx coupon example below:
Basaglar brand name is most expensive