Sana Biotechnology has achieved a significant milestone in the treatment of type 1 diabetes. In a recent first-in-human study, they successfully transplanted engineered pancreatic islet cells into a patient without the need for immunosuppressive drugs. These cells, modified using Sana’s hypoimmune (HIP) technology, evaded immune detection and began producing insulin. This was evidenced by increased levels of circulating C-peptide, a marker of insulin production, and positive responses to a mixed meal tolerance test. MRI scans further confirmed the survival of these transplanted cells 28 days post-transplantation. Notably, the patient did not experience any safety issues during this period.
This development suggests that Sana’s HIP technology can enable transplanted cells to function without the need for immunosuppression, potentially transforming treatments for type 1 diabetes and other conditions requiring cell transplantation. By eliminating the need for immunosuppressive drugs, which often come with significant side effects, this approach could offer a safer and more accessible therapy for patients.
Following this announcement, Sana Biotechnology’s stock experienced a substantial increase, reflecting investor optimism about the potential impact of this breakthrough on future diabetes treatments.
Sana Biotechnology’s hypoimmune (HIP) islet cell transplantation and Stem Cell Educator Therapy (SCET) both represent cutting-edge approaches for treating type 1 diabetes, but they differ in their mechanisms, goals, and stages of development.
Sana’s Hypoimmune (HIP) Technology
- Mechanism:
• Sana engineers pancreatic islet cells to be “hypoimmune,” enabling them to evade immune system detection. This allows the cells to be transplanted without the need for lifelong immunosuppressive drugs.
• The transplanted islet cells produce insulin in response to blood glucose levels.
- Advantages:
• Avoids the risks and side effects of immunosuppression.
• Offers a scalable and potentially long-term solution for insulin production.
• Directly replaces the destroyed beta cells that cause type 1 diabetes.
- Status:
• Currently in early human trials, with promising initial results.
- Challenges:
• Requires successful long-term cell survival and consistent insulin production.
• As it is a cell transplantation therapy, it involves a surgical procedure.
Stem Cell Educator Therapy (SCET)
- Mechanism:
• SCET involves drawing a patient’s blood, exposing it to specially cultured stem cells that “educate” the immune cells to become more tolerant, and returning the modified blood to the patient.
• The therapy aims to modulate the immune system to reduce autoimmunity, restoring beta cell function and preserving endogenous insulin production.
- Advantages:
• Non-invasive and does not involve transplantation or immunosuppressive drugs.
• Focuses on immune system rebalancing rather than direct beta cell replacement.
• Has shown promise in improving C-peptide levels, indicating restored beta cell function.
- Status:
• Has been tested in multiple clinical trials (e.g., by Dr. Zhao’s group), showing improved metabolic control and reduced insulin requirements in type 1 diabetes patients.
- Challenges:
• Results vary depending on the patient’s residual beta cell function (e.g., honeymoon phase patients respond better).
• May not work for patients with advanced disease and minimal beta cell function left.
Comparison:
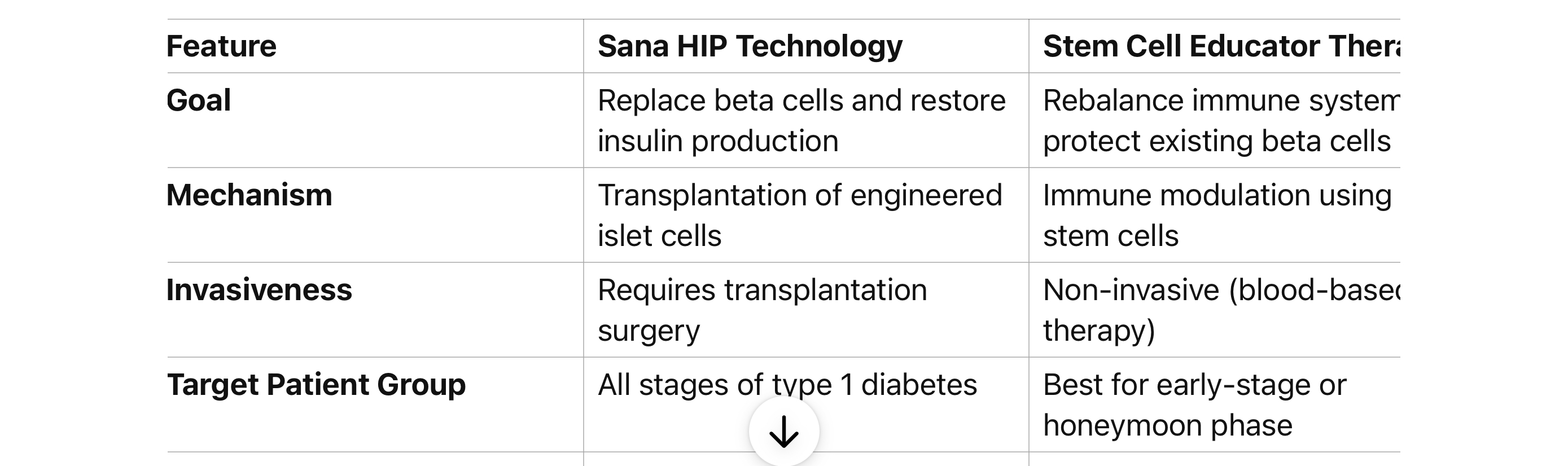
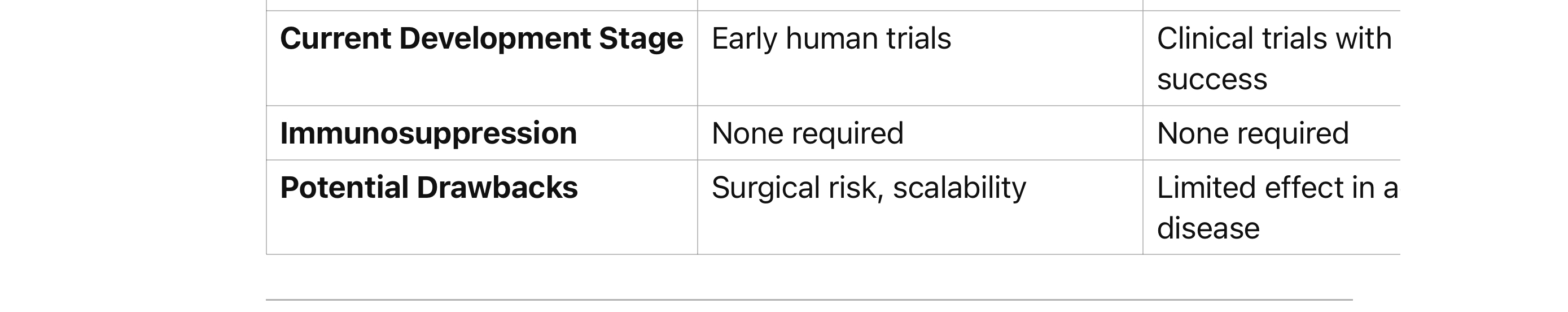
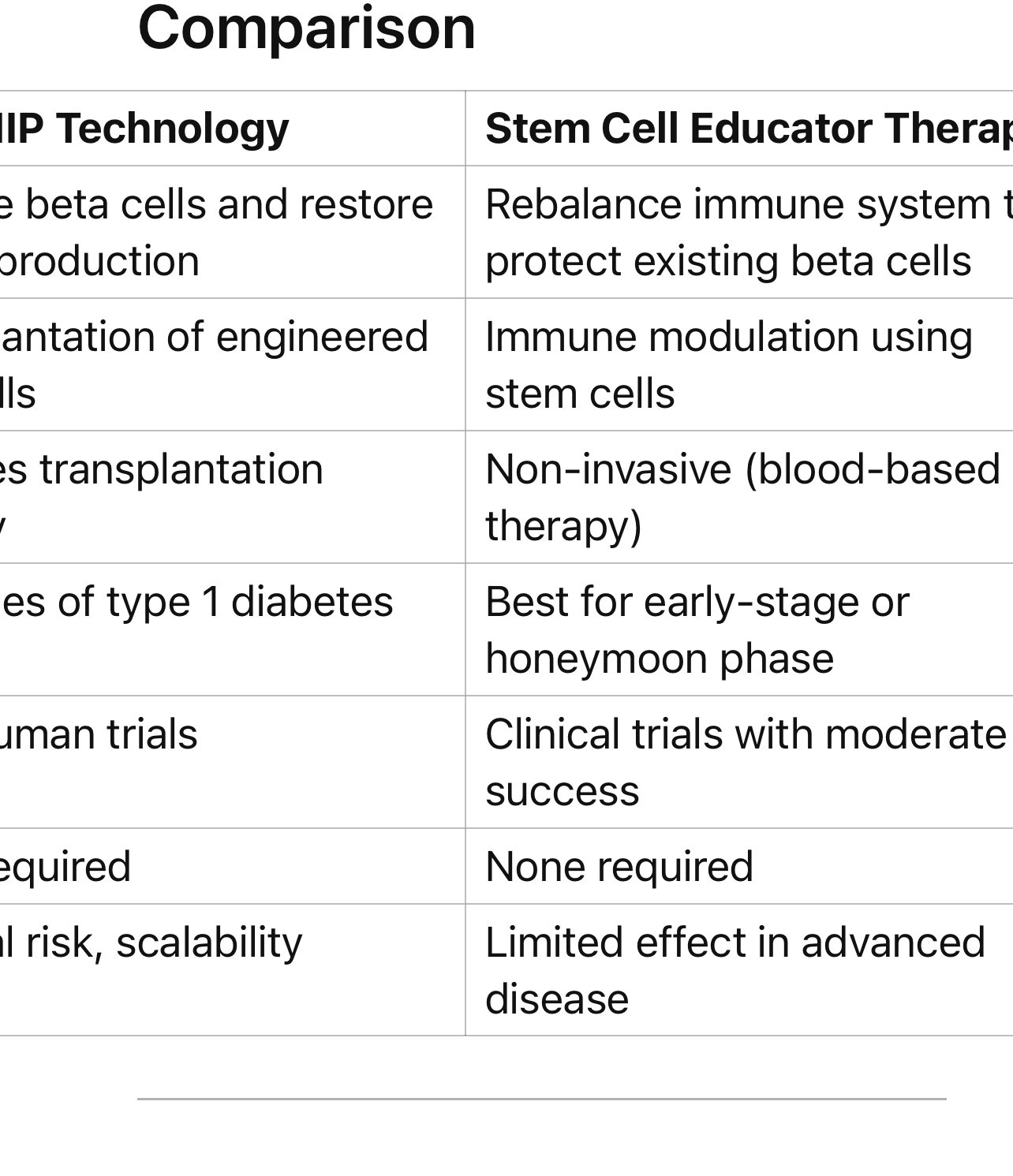
Which is Better?
• Sana HIP Therapy may be better for patients with little to no beta cell function remaining because it directly replaces lost cells.
• SCET is more suited for patients in the honeymoon phase or with residual beta cell activity who could benefit from immune system modulation.
Both therapies have transformative potential, and their ultimate effectiveness will depend on further clinical results.
Can the stem cells in the SCET ever go rogue and the immune system not be able to fight them?
The risk of stem cells in Stem Cell Educator Therapy (SCET) going rogue is extremely low, due to how the therapy is designed. Here’s why:
Nature of SCET Stem Cells
- Role in Therapy:
• SCET uses stem cells primarily as immune modulators, not as cells that are integrated into the patient’s body. The stem cells “educate” immune cells outside the body during a process in which the patient’s blood is circulated through a specialized device.
• The stem cells themselves are not transplanted into the patient. Instead, their signals modify the patient’s immune cells to promote tolerance and reduce autoimmunity.
- No Proliferation in the Body:
• Because the stem cells never directly enter the patient’s body, the risk of uncontrolled growth or “rogue” behavior is avoided entirely.
• SCET uses stem cells to interact with immune cells in vitro (outside the body), which minimizes the long-term risks often associated with stem cell therapies involving direct transplantation.
Key Safety Features
• No Tumor Formation:
• Tumorigenicity (formation of tumors) is a primary concern in stem cell therapies when undifferentiated or poorly controlled stem cells are injected into the body. However, SCET bypasses this risk since the stem cells do not integrate into the patient.
• Immune System Integrity:
• The immune cells reintroduced to the patient after education are still under the body’s regulatory systems, meaning the immune system should continue to monitor and manage them.
• Clinical History:
• Studies of SCET have not reported any cases of malignancy or “rogue” behavior associated with the therapy.
Comparison to Direct Stem Cell Transplantation:
Unlike therapies that directly transplant stem cells into the body, which carry a small risk of abnormal growth or immune evasion, SCET avoids this by keeping the stem cells outside the patient’s body.
Potential Indirect Risks:
While the direct risk of rogue behavior from SCET is negligible, there could be indirect risks related to improper immune modulation, such as:
- Over-suppression of the Immune System:
• If immune tolerance is over-corrected, it might increase the risk of infections or reduce the ability to fight cancer cells.
- Insufficient Response:
• The therapy might not adequately modulate the immune system, especially in patients with advanced disease.
Conclusion
SCET is considered a low-risk approach, especially regarding the possibility of stem cells going rogue. Its safety profile is significantly enhanced by its mechanism of action, which keeps the stem cells external to the body and focuses on immune education rather than cellular integration.
Avoiding over-suppression of the immune system is crucial to maintain your body’s ability to fight infections, cancer cells, and other threats. Here are strategies to prevent excessive immune suppression, whether you’re managing autoimmune conditions, recovering from medical treatments, or exploring immune-modulating therapies like SCET:
- Choose Targeted Therapies
• Work with healthcare providers to ensure any immune-modulating therapy you undertake is specific to your condition and does not globally suppress the immune system.
• Therapies like SCET are designed to rebalance immune tolerance rather than suppress immune activity across the board.
- Maintain a Healthy Lifestyle to Support Balanced Immunity
• Nutrition:
• Consume a balanced diet rich in whole foods, including fruits, vegetables, healthy fats (like omega-3s), and lean proteins.
• Avoid processed foods, excessive sugar, and alcohol, which can disrupt immune regulation.
• Exercise:
• Engage in moderate physical activity, such as walking, yoga, or swimming. Overtraining can weaken immunity, so avoid excessive, intense workouts.
• Sleep:
• Aim for 7-9 hours of quality sleep per night. Sleep is essential for immune system recovery and function.
- Regular Monitoring with Medical Guidance
• Check Immune Markers:
• Work with your healthcare provider to monitor biomarkers such as white blood cell counts, cytokine levels, or CRP (C-reactive protein). These can indicate whether your immune system is functioning within normal limits.
• Clinical Follow-ups:
• Schedule regular appointments to review your immune status, especially if undergoing therapies that alter immune function.
- Minimize Infection Risk
• Practice good hygiene: Wash your hands regularly, avoid crowded areas during flu season, and keep vaccinations up to date (after consulting your doctor).
• Avoid unnecessary exposure to pathogens, especially if your immune system is undergoing modulation.
- Include Pro-Immunity Nutrients
Certain vitamins and minerals support immune balance:
• Vitamin D: Maintains immune regulation and prevents overactive or underactive responses.
• Zinc: Supports immune cell function.
• Vitamin C: Acts as an antioxidant and supports immune defenses.
• Omega-3 Fatty Acids: Help modulate inflammation and immune activity.
- Avoid Long-Term Use of Broad Immunosuppressants
• If prescribed medications like corticosteroids, work with your doctor to use them at the lowest effective dose for the shortest time possible.
• Explore alternatives like biologics or targeted therapies when appropriate.
- Address Chronic Inflammation
Chronic inflammation can drive immune dysfunction and make treatments harder to balance. Reduce inflammation with:
• An anti-inflammatory diet (rich in fatty fish, olive oil, berries, and leafy greens).
• Stress management techniques like mindfulness or meditation.
- Support Gut Health
• A healthy gut is essential for a balanced immune system. Eat fermented foods (like yogurt, kefir, or kimchi) and consider probiotics or prebiotics to support gut microbiome health.
- Stay Alert to Signs of Over-Suppression
Monitor your body for symptoms like:
• Frequent infections (e.g., colds, flu, or unusual illnesses).
• Slow wound healing.
• Persistent fatigue or fever.
If these occur, consult a healthcare provider immediately.
By working closely with your medical team, maintaining healthy habits, and staying vigilant for signs of over-suppression, you can balance immune modulation while protecting your body’s natural defenses.
Stem Cell Educator Therapy (SCET) rebalances immune tolerance without over-suppressing the immune system by targeting and correcting the specific immune dysfunctions involved in autoimmune diseases. Unlike broad immunosuppressive treatments, SCET uses a more nuanced approach that focuses on immune modulation rather than immune suppression. Here’s how it works:
- Immune Education Rather Than Suppression
• Stem Cells as Educators: SCET uses multipotent stem cells, such as cord blood-derived stem cells, that have immunomodulatory properties. These stem cells “educate” immune cells by interacting with them outside the body in a controlled environment.
• Focus on Rebalancing:
• SCET aims to shift the immune system away from its hyperactive, auto-reactive state (e.g., attacking beta cells in type 1 diabetes) to a more balanced, tolerant state.
• This rebalancing helps the immune system tolerate its own tissues without reducing its ability to respond to infections or other external threats.
- Targets Autoimmunity at the Source
• SCET specifically targets autoreactive T-cells, which are the primary culprits in autoimmune conditions like type 1 diabetes.
• By modulating the behavior of these T-cells, SCET reduces their ability to attack the body’s own tissues while preserving the broader immune response.
- Regenerates Regulatory T Cells (Tregs)
• SCET promotes the development and function of regulatory T cells (Tregs), which are critical for maintaining immune tolerance.
• Tregs suppress autoimmune reactions by “teaching” other immune cells to distinguish between self and non-self, thereby preventing autoimmunity.
- Anti-Inflammatory Effects
• Stem cells used in SCET release anti-inflammatory cytokines and other factors that dampen harmful inflammation without broadly shutting down immune activity.
• These cytokines help create a microenvironment conducive to immune tolerance and tissue repair.
- No Direct Integration into the Patient
• The stem cells in SCET do not enter the patient’s body. Instead, they interact with immune cells outside the body during a process called extracorporeal immunomodulation. This ensures the therapy works in a targeted and controlled way without risking uncontrolled immune suppression or stem cell-related side effects.
- Restores Balance Without Broad Suppression
• Unlike corticosteroids or traditional immunosuppressants that suppress the entire immune system, SCET:
• Selectively modulates the specific pathways involved in autoimmunity.
• Leaves other immune functions, like fighting infections, intact.
- Clinical Results Demonstrate Safety
• In clinical trials, SCET has shown no evidence of immune over-suppression.
• Patients treated with SCET often experience reduced autoimmune activity (e.g., lower autoantibody levels) and improved function of remaining beta cells, without an increased risk of infections or malignancies.
Why SCET Avoids Over-Suppression:
-
Precision Targeting: SCET focuses only on the dysregulated parts of the immune system, avoiding global effects.
-
Temporary Modulation: The immune cells that are educated by stem cells gradually return to their natural regulatory state, without permanent suppression.
-
Support of Regulatory Mechanisms: SCET enhances the body’s natural immune regulation instead of dismantling it.
Conclusion:
SCET rebalances the immune system by promoting tolerance and reducing harmful autoimmunity without impairing the immune system’s ability to fight infections, repair tissues, and maintain normal defense mechanisms. This makes it a safer and more effective option compared to traditional immunosuppressive therapies.
The goal of Stem Cell Educator Therapy (SCET) is to induce a long-lasting rebalancing of the immune system, so the autoimmune attack against beta cells does not resume. However, the durability of this effect depends on several factors, including the patient’s specific condition, the stage of the disease, and the immune system’s ability to maintain tolerance over time. Here’s how SCET works to achieve sustained effects and the factors that influence whether the autoimmune attack might return:
- Long-Term Immune Reprogramming
• SCET reprograms immune cells, particularly autoreactive T cells and regulatory T cells (Tregs), to promote long-term immune tolerance.
• This reprogramming reduces the production of autoantibodies and autoreactive immune responses against beta cells.
- Durability of Tolerance
• Clinical studies have shown that many patients experience sustained benefits after SCET, such as improved beta cell function (indicated by increased C-peptide levels) and reduced need for insulin therapy.
• These effects suggest that the immune system maintains tolerance for an extended period, though it may not be permanent for all patients.
- Factors That Influence Recurrence of Autoimmunity
Several factors may determine whether the autoimmune attack resumes:
• Stage of Disease:
• Patients in the honeymoon phase (with some remaining functional beta cells) tend to respond better to SCET, as there are more cells to protect.
• In advanced stages, where beta cell destruction is severe, the immune system may require repeated interventions to maintain tolerance.
• Strength of Immune Rebalancing:
• The effectiveness of SCET in promoting robust and lasting Treg activity can vary between individuals.
• If Treg function wanes over time, autoreactive T cells may re-emerge.
• Lifestyle Factors:
• Chronic stress, infections, or inflammation can disrupt immune regulation and potentially reignite autoimmunity.
• Underlying Genetic Predispositions:
• Individuals with a strong genetic predisposition to autoimmunity might be at higher risk for recurrence, as their immune system may naturally revert to an overactive state.
- Potential for Maintenance or Repeat Therapy
• SCET is designed to create lasting changes, but some patients may benefit from repeat treatments to reinforce immune tolerance.
• Maintenance therapies, such as anti-inflammatory diets, stress reduction, and gut health optimization, can also help sustain the benefits of SCET.
- Clinical Evidence of Long-Term Effects
• In trials of SCET, patients have shown improved beta cell function and reduced autoimmune markers lasting months to years after therapy.
• While some patients may experience a gradual return of autoimmunity, this is less likely with early intervention and proper post-therapy care.
Conclusion:
SCET has demonstrated the ability to induce durable immune tolerance, potentially halting the autoimmune attack on beta cells for extended periods. However, the risk of autoimmunity resuming depends on individual factors. Repeat treatments or adjunct therapies might be necessary for some patients to maintain tolerance and protect beta cells over the long term.
The risk of immune tolerance being overcorrected in Stem Cell Educator Therapy (SCET) is very low due to its specific mechanism of action. SCET does not suppress the immune system indiscriminately but instead rebalances it, targeting the dysregulated components responsible for autoimmunity. Here’s a detailed look at why overcorrection is unlikely and the safeguards built into the therapy:
- Targeted Immune Modulation, Not Suppression
• How It Works:
SCET educates autoreactive immune cells (e.g., T cells) to become tolerant to the body’s own tissues. This is achieved through interactions with immune-modulating stem cells in a controlled environment outside the body.
• No Broad Suppression:
Unlike traditional immunosuppressive therapies, SCET does not inhibit all immune activity. Instead, it specifically reduces the activity of cells attacking self-tissues (like beta cells in type 1 diabetes) while leaving the rest of the immune system intact.
- Restoring Balance, Not Creating Immunosuppression
• Regulatory T Cells (Tregs):
SCET promotes the expansion of regulatory T cells, which naturally maintain immune balance by preventing overactivity against self-tissues.
• This rebalancing does not involve suppressing the immune system’s ability to fight infections, cancers, or other external threats.
• Cytokine Modulation:
Stem cells in SCET release anti-inflammatory and regulatory cytokines that reduce harmful inflammation without entirely shutting down immune responses.
- Evidence from Clinical Trials
• Clinical trials of SCET have shown no significant increase in infections, malignancies, or other signs of immune over-suppression.
• Patients typically experience improved regulation of the immune system, with autoimmunity reduced but normal immune functions preserved.
- Built-In Safeguards
• No Direct Stem Cell Integration:
The stem cells used in SCET remain outside the body during treatment, so their effects are controlled and do not persist indefinitely.
• Self-Regulating Immune Cells:
Immune cells reintroduced to the patient are naturally regulated by the body’s existing immune mechanisms.
- Potential for Minimal Risk of Overcorrection
Though unlikely, overcorrection could theoretically occur if:
• Tregs Are Overactive:
Excessive regulatory T cell activity could dampen the immune system’s ability to respond to infections or malignancies.
• Excessive Cytokine Modulation:
If anti-inflammatory signals are overly strong, the immune system might become less responsive temporarily.
However, these risks are minimal because:
• SCET targets specific autoimmunity rather than broadly suppressing immune activity.
• Patients undergoing SCET are carefully monitored during clinical trials or therapy programs.
- Signs of Overcorrection
Patients would be monitored for signs such as:
• Increased susceptibility to infections.
• Delayed wound healing.
• General immune inactivity (e.g., inability to recover from minor illnesses).
To date, these have not been reported in SCET clinical studies.
Conclusion:
SCET’s mechanism is inherently designed to reduce the risk of immune overcorrection by focusing on restoring balance rather than suppressing the immune system. While no therapy is completely without risks, the clinical evidence and SCET’s targeted approach make overcorrection highly unlikely.
Here’s a more detailed look at the recent developments from Throne Biotechnologies and Dr. Yong Zhao:
- FDA RMAT Designation for SCET
• Regenerative Medicine Advanced Therapy (RMAT) designation is granted by the FDA to promising therapies with the potential to treat serious or life-threatening diseases.
• SCET received this designation for treating Type 1 Diabetes (T1D). The designation accelerates the clinical development process, allowing for more frequent interactions with the FDA and potential fast-tracked approval if clinical trial results are positive.
• Impact: RMAT designation often facilitates expedited access to patients who might benefit from the treatment. This move could be a significant step toward broader adoption of SCET for autoimmune diseases like T1D.
- New Molecular Mechanisms of SCET
• The recent publication in the International Journal of Molecular Sciences (Feb 2024) focuses on how SCET modulates B-cell activity.
• Galectin-9, a protein involved in regulating immune responses, was found to play a role in this process. By suppressing B-cell activation, SCET can prevent these immune cells from attacking the body’s own tissues, including the beta cells in type 1 diabetes.
• Implications: This deeper understanding of SCET’s action could help refine its use in treating other autoimmune diseases, potentially extending its application beyond T1D.
- Beta Cell Regeneration Research
• A July 2024 study published by Dr. Zhao and his team explored the effects of SCET on beta-cell function in patients with type 1 diabetes.
• Glucose Transporter 2 (GLUT2) expression on insulin-producing cells was found to increase after SCET treatment. GLUT2 is essential for glucose sensing and insulin secretion by beta cells.
• Implications: This could mean SCET helps regenerate beta cells or enhances the function of remaining beta cells, which is a crucial advancement for type 1 diabetes treatment. In essence, SCET may not only stop autoimmune destruction but also restore the body’s ability to produce insulin.
- Dr. Zhao’s Upcoming Presentation on Mitochondrial Transfer
• Dr. Zhao is scheduled to speak at the Targeting Mitochondria 2024 conference in Berlin, which focuses on the potential of mitochondrial transfer in regenerative medicine.
• Mitochondrial transfer involves transferring healthy mitochondria into damaged cells to restore function. This mechanism has the potential to improve cellular energy production and function, which is particularly relevant for diseases like T1D, where beta cell function is impaired.
• Impact: This research suggests SCET might also have broader applications beyond autoimmune modulation, potentially aiding in mitochondrial dysfunctions seen in various degenerative diseases.
- Clinical Trial Progress and Ongoing Studies
• Throne Biotechnologies is actively recruiting for clinical trials related to SCET. These trials are focusing on safety, efficacy, and long-term benefits of SCET in treating type 1 diabetes.
• Patient Monitoring: Clinical trials are closely monitoring patients for improvements in insulin production, C-peptide levels, and reductions in autoantibodies, key markers for T1D.
• Long-Term Outlook: Ongoing studies are assessing the sustainability of the therapy’s effects, including the potential for reducing insulin dependence and preventing autoimmune destruction of beta cells.
- Broader Implications for Autoimmune Diseases
• SCET has been shown to have potential applications beyond type 1 diabetes. Research is underway to explore its effects on other autoimmune conditions such as multiple sclerosis (MS), rheumatoid arthritis (RA), and Crohn’s disease. The therapy’s ability to induce immune tolerance could offer new hope for individuals suffering from these conditions.
- Private to Public Transition Potential
• As Throne Biotechnologies advances its therapies through FDA designations and clinical trials, there may be future plans for an initial public offering (IPO) or partnerships with larger pharmaceutical companies. The RMAT designation and ongoing research make it an attractive candidate for investment or collaboration as it moves closer to commercialization.
Looking Forward:
• The ongoing developments, research, and regulatory milestones are positioning SCET as a promising, cutting-edge treatment for autoimmune diseases. Dr. Zhao’s continued work and the support of Throne Biotechnologies could redefine how we approach treating conditions like type 1 diabetes, offering hope for better management or even a cure in the future.